Hospital Acquired Pressure Injuries (HAPI, formally pressure ulcers) can result in a lifetime of pain, suffering and even possibly death for the patient. HAPI rates are reported to the National Database of Nursing Quality Indicators (NDNQI) which is the, “Only national, nursing quality measurement program that provides hospitals with unit-level performance comparison reports (NDNQI, 2010b, p. 2). Healthcare leadership can use the information provided by the NDNQI to establish organizational goals for improvement at the unit level and mark progress in improving patient care and the work environment.
The NDNQI categorizes the HAPI as an outcome-specific Nursing Sensitive Indicator (NSI). NSIs are measures and indicators that reflect the structure, processes and outcomes of nursing care (American Nurses Association, 2004). In other words, a health care facility’s yearly HAPI occurrence is a direct reflection on the quality of nursing care provided at that facility.
Stage III and IV HAPIs are defined as “never events” by the Center of Medicare & Medicaid Services (CMS). In October 2008, stage III and IV HAPIs became non-CMS reimbursable, and HAPI expenses became out of pocket expenses for health care systems. Padula and Delarmente report that, “U.S. HAPI costs could exceed $26.8 billion. About 59% of these costs are disproportionately attributable to a small rate of Stage III and IV pressure injuries and full-thickness wounds that occupy clinician time and hospital resources.”
Perioperative pressure injuries can increase the cost of surgery-related hospital stays by an estimated 44% and may add approximately $1.3 billion annually to health care costs in the United States (Spector, Limcangco, Owens, Steiner 2016).
Perioperative related HAPIs can take up to 48-72 hours to appear (Hayse, Spear and Lee et al. 2015) and can be difficult to track so many times perioperative HAPI’s are attributed to the wrong phase of care. Perioperative leadership and staff can fall into the, “out of sight out of mind” thought process because they never see the poor outcomes that occur with HAPIs. Surgical Services can play a key role in decreasing HAPIs. The perioperative phase of care is the first care to touch the patient and thus can be the first line of defense against HAPIs.
The surgical patient presents itself with a unique set of intrinsic (co-morbidities) and extrinsic (surgical environment) risk factors that increases the surgical patient’s risk for a perioperative pressure injury. Each phase of perioperative care has its own set of risk factors that should be addressed and mitigated in that phase of care, with the implementation of evidence-based interventions.
Opportunities to decrease HAPIs starts upon admission to the preop area with a thorough head-to-toe preop skin assessment. The preop skin assessment can identify present on admission (POA) pressure injuries. This is important because if a stage I or II progresses into a stage III or IV pressure injury during the hospitalization, CMS will not reimburse any associated cost. Finding a POA also gives the preop nurse an opportunity to implement interventions so that the injury does not progress. One extrinsic risk in the preop area is due to the extended time they may be laying on the stretcher. This can cause pressure and shear forces that are the foundation for a pressure injury. Oomes states that, “Although ischemic injury occurs slowly, shear causes deformation and tissue destruction within minutes to hours; and Brienza recommends that, prevention interventions also should focus on preventing shear, not just prolonged pressure.”
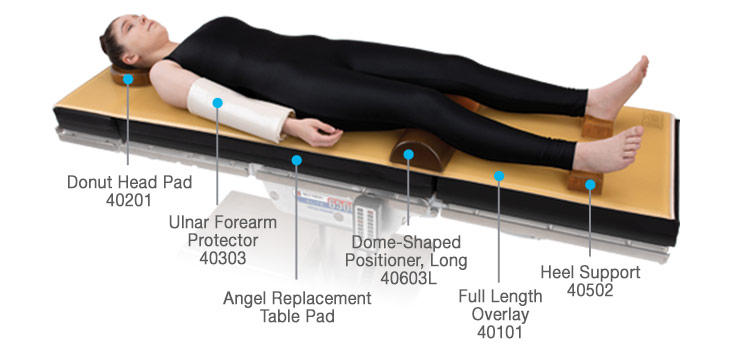
Evidence-based interventions that can be implemented to prevent shear and pressure are in the application of a five-layer soft silicone border foam dressing on the “high risk “areas (heels, sacra) (Kimsey 2019) and offloading the pressure by encouraging the patients to move. A detailed hand off communication between the preop nurse and the OR nurse should include the skin assessment, risk assessment and the skin injury preventions that have already been put into place. A perioperative specific risk assessment tool should be used to identify the “at risk” for pressure injury patient in all three phases of perioperative care.
Decreasing HAPIs within your health care system not only decreases cost it decreases poor patient outcomes. The implementation of pressure injury prevention interventions in the three phases of surgical care will reduce HAPIs. It takes leadership support and the collaboration of frontline nurses (in all phases of care), to successfully implement a Perioperative Pressure Injury Reduction Plan.
Stay tuned for next time where we will discuss the risks and interventions for the Interop phase of care.
Brienza D. Ischemia and deformation: two damage mechanisms leading to deep tissue pressure injuries. Presented at: The National Pressure Ulcer Advisory Panel 2018 Annual Conference; March 2-3, 2018; Las Vegas, NV.

