Nursing shortages, burnout and compassion fatigue require nurses to practice self-care.
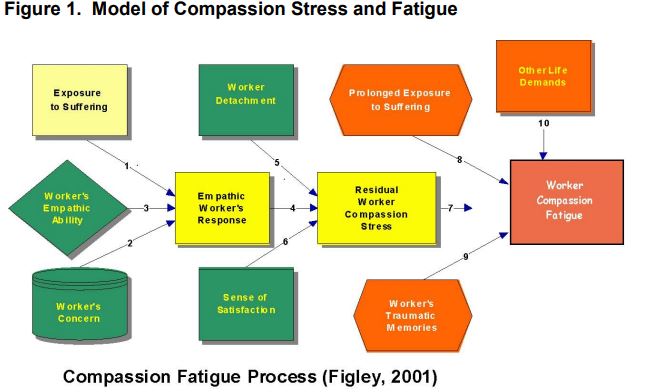
Compassion Fatigue can occur with exposure to one case or can be due to a “cumulative” level of trauma. Compassion fatigue develops over time, taking weeks, sometimes years to surface. It is a low level, chronic clouding of caring and concern for others. Over time, the ability to feel and care for others becomes eroded through overuse of the skills of compassion.
Emotional blunting may occur, whereby reactions to situations are different than one would normally expect. Reflecting on practice over the last year can help identify if compassion fatigue or burn out has negatively impacted job our satisfaction or patient care.
Some symptoms of compassion fatigue affects many dimensions of well-being such as:
- Nervous system arousal (sleep disturbance)
- Increases in emotional intensity
- Decreases in cognitive ability
- Impairment in behavior and judgment
- Self-isolation and loss of morale
- Loss of self-worth and emotional modulation
- Identity, worldview, and spirituality impacted
- Beliefs and psychological needs – safety, trust, esteem, intimacy, and control
- Loss of hope and meaning = existential despair
- Anger toward perpetrators or causal events
http://www.figleyinstitute.com/documents/Workbook_AMEDD_SanAntonio_2012July20_RevAugust2013.pdf
Reflection
Reflection is the process needed to gain insight into professional practice by thinking analytically about the elements of practice. The insights developed, and lessons learned from reflection and applied to our practice only enhances it. Reflecting on the uncertain times we live in today, where the “new normal”, has become “normal” and ambivalence and compassion hold hands. In 2022 what can we as nurses, learn from the insights gained over this past year that can rejuvenate our health and our practice?
Healthcare professionals enter the field because they care about people and want to support their patients’ health and wellbeing. When patients experience pain and fear, healthcare professional respond with empathy and care for the patient and family. Healthcare professionals feel satisfaction from making a positive contribution to their patients’ health.
Front line workers are still positively impacting patients’ lives every day, but the overall satisfaction is waning. The bravery and dedication of America’s frontline workers have been displayed on front-page newspaper stories across the country throughout the pandemic. However, the pandemic has also been a huge strain on nurses and the healthcare system, due in part to limited staff and resources.
Specific data for nursing shortages that have been caused by the COVID-19 pandemic are not yet available, but there is anecdotal evidence that caring for COVID patients in such unrelenting numbers is leading to stress, burnout, resignations, and retirements. Nurse burnout involves the emotional and physical exhaustion that comes with the stressful responsibilities required for nursing. In comparison, compassion fatigue results when prolonged emotional strain culminates in detachment and difficulties in providing empathetic care. Compassion fatigue is different than burn out, it’s also called “vicarious traumatization” or secondary traumatization. The emotional residue or strain of exposure to working with those suffering from the consequences of traumatic events. Nurse burnout and compassion fatigue are different, but they can co-exist.
Lastly, another factor contributing to nurse burnout is the nationwide nursing shortage in the U.S. The Bureau of Labor Statistics projects that the number of registered nurses could increase from 3 million in 2019 to 3.3 million a decade later. That’s an increase of about 7.2%., the demand for nurses will outpace the supply. This undoubtedly will add another level of stress to an already overburdened healthcare system.
“Reflection allows you to identify and appreciate positive experiences and better identify ways that you can improve your practice and service delivery. It can also be useful when you have had more challenging experiences; helping you to process and learn from them.” (HPCP, Health and Care Professions Council, https://www.hcpc-uk.org/standards/meeting-our-standards/reflective-practice/what-is-reflection/)

Preventative strategies, like self-care and reflection can help combat compassion fatigue and burn out. Bringing back the compassion to practice in 2022 may seem like a daunting task, prioritizing self-care is the first step.
References
https://www.hcpc-uk.org/standards/meeting-our-standards/reflective-practice/what-is-reflection/
https://www.stress.org/military/for-practitionersleaders/compassion-fatigue
https://online.marymount.edu/blog/nursing-shortage-statistics
https://nursejournal.org/resources/nurse-burnout/
https://www.aacnnursing.org/news-information/fact-sheets/nursing-shortage