Preventing Hospital-Acquired Pressure Injuries in 2026: Perioperative Strategies to Avoid CMS Never Events
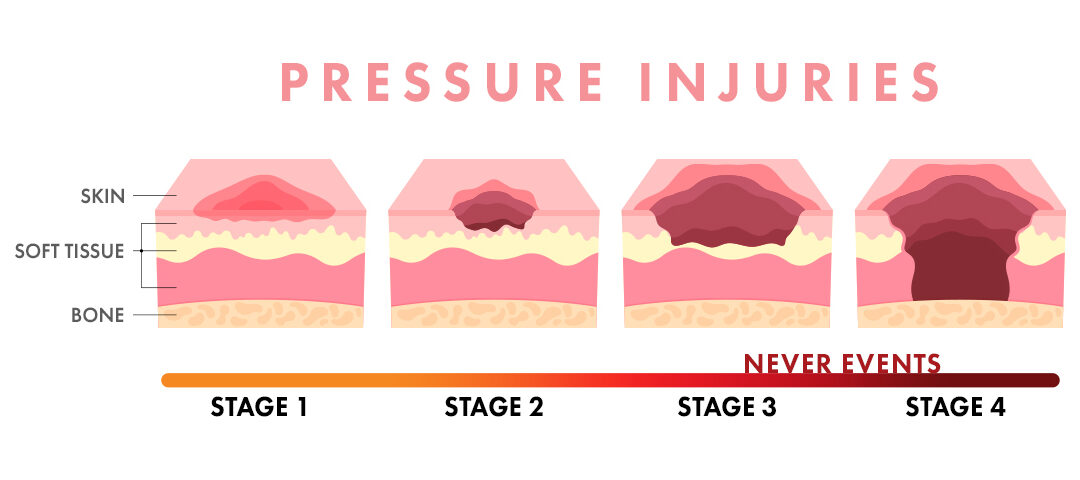
Hospital-Acquired Pressure Injuries (HAPIs) remain a costly and preventable harm. The Centers for Medicare & Medicaid Services (CMS) still classifies Stage III and IV HAPIs as “never events.” Stage III and IV HAPIs are not reimbursable, making the costs the responsibility of health care systems.
Earlier studies estimated HAPIs cost more than $26.8 billion each year. Recent models show an average cost of about $18,000 per injury. About 59% of these expenses are disproportionately attributable to a small rate of Stage III and IV full-thickness wounds that demand significant clinical time and hospital resources.” Pressure injury prevention remains a top clinical and financial priority for all hospitals.
Never events increase financial risk for facilities
The 2025 Hospital Acquired Conditions (HAC) Reduction Program penalizes facilities ranking in the lowest quartile for HAC performance. These penalties increase financial risk for organizations.
Nursing Quality Indicators and National Benchmarking
HAPI rates remain a key nursing-sensitive outcome that are tracked through the National Database of Nursing Quality Indicators (NDNQI). NSIs are measures and indicators that reflect the structure, processes and outcomes of nursing care. NDNQI contains more than 250 validated nursing measures so many hospitals use NDNQI data for quality improvement and Magnet® alignment. In other words, a health care facility’s yearly HAPI occurrence is a direct reflection on the quality of nursing care provided at that facility.
Pressure injuries cause pain and disability, as well as a higher risk of death. HAPIs reflect gaps in nursing care. Because hospital-acquired pressure injuries are Nursing Sensitive Indicators, they show how well nurses assess risk and protect the skin. Surgical Services can play a key role in decreasing HAPI “never events.” Strong prevention programs can improve both patient outcomes and organizational performance.
Cost and Risk of Perioperative Pressure Injuries
Perioperative pressure injuries add major cost to surgical care. Research shows they increase surgical stay costs by 44% and they add about $1.3 billion in national costs each year. (Spector, Limcangco, Owens, and Steiner 2016).
Many intraoperative pressure injuries do not manifest immediately and may appear 48 to 72 hours after surgery. This delayed presentation makes it challenging to identify the true cause. Many pressure injuries that start in the OR are frequently misattributed to the inpatient phase of care. This creates an “out of sight, out of mind” effect for surgical teams. As a result, perioperative staff may not see the final injury, even though it began during surgery.
Perioperative Pressure Injury Risk Factors
Patients in surgery face unique risks. These include intrinsic (co-morbidities) and extrinsic (surgical environment) factors. These factors increase the surgical patient’s risk for a perioperative pressure injury. Each phase of perioperative care presents specific risk factors, which should be mitigated using evidence-based interventions.
Intrinsic Risk Factors
- Diabetes
- Obesity or low BMI
- Vascular disease
- Older age
- Poor nutrition
- Limited mobility
- Chronic illness
Extrinsic Risk Factors
- Long surgical time
- Prone or lateral positioning
- Poor padding
- Rigid surfaces
- Heat and moisture
- Shear forces
- Device-related pressure
Recent perioperative literature confirms that extrinsic procedure-related factors significantly contribute to intraoperative pressure injuries (IAPI). IAPI refers to position-related tissue injury that occurs within 72 hours after surgery. For example, a 2024 study found that body position, longer operative time, and higher BMI independently predicted intraoperative pressure injury. Another cohort study demonstrated that prone positioning nearly tripled the risk of IAPI compared to non-prone positions.
Importance of Preoperative Skin Assessment
A full preoperative skin assessment helps identify present-on-admission injuries. This protects hospitals from incorrect HAPI classification and helps nurses plan early interventions.
Opportunities to decrease HAPIs start upon admission to the preop area with a thorough head-to-toe preoperative skin assessment. The preop skin assessment can identify present on admission (POA) pressure injuries. This is important because if a stage I or II progresses into a stage III or IV “never event” during the hospitalization, CMS will not reimburse any associated cost.
CMS does not currently deny payment for Stage II HAPIs. However, Stage II injuries are being added to harm tracking systems. Penalties may begin as early as 2027 so accurate assessments and documentation is essential.
Evidence-Based Interventions to Prevent HAPIs in Surgery
- Use Protective Foam Dressings
Five-layer silicone border dressings help lower pressure and shear. These dressings are most effective on the heels and sacrum, and research supports their use for high-risk surgical patients. - Improve Positioning and Offloading
Offload all bony areas and use gel or viscoelastic pads. Remove any tubing beneath the patient and recheck the position often. Intraoperative micro-movements and frequent small adjustments can help mitigate the risk. - Use a Perioperative Risk Tool
A perioperative-specific tool helps identify risk and should be used in all phases of surgical care. This includes preoperative, intraoperative, and postoperative periods. The Braden Scale is not a validated risk assessment tool for the surgical patient. - Strengthening Team Communication
Good hand-off communication is essential which includes teams sharing risk scores, dressings used, and skin findings. These important steps support continuity of care. - Engage Nursing and Organizational Leadership
Leadership support drives lasting change. Teams need education, clear workflows, and shared accountability. Collaboration between units is essential for success.
Preventing hospital-acquired pressure injuries is essential for safe, high-quality care. The perioperative phase carries high risk but also offers major pressure injury prevention opportunities. When teams use evidence-based strategies, many injuries can be avoided. Better prevention leads to fewer CMS “never events,” lower cost, and better patient outcomes.
Our proprietary Akton® polymer reduces the risk of pressure injuries
The ultrasoft polymer combined with the soft, flexible surface of our pads allows the product to move with the patient, reducing negative effects of shear on fragile skin. In addition, the Akton® polymer distributes weight and dissipates heat; reducing the risk of high-pressure points and hot spot development that can lead to pressure injuries. These combined benefits enhance patient protection.
B9053-000